Rest, Purpose, and Revitalization
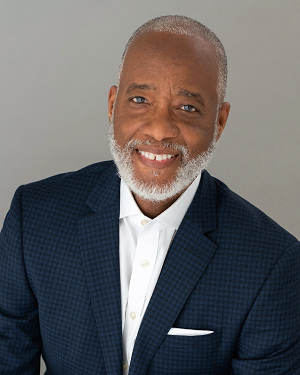
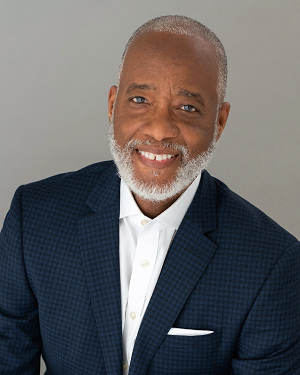
David E. Conroy, PhD, SBM President
 David E. Conroy, PhD
David E. Conroy, PhD
SBM President
With Thanksgiving in the rearview mirror and the New Year in sight, it is a good time to reflect on the year that passed and the year that lies ahead. Suffice it to say, 2021 has been exhausting. I have been grateful for all of the SBM volunteers, leaders, and staff who have plowed ahead to make sure SBM is creating value for members all year round. I marvel at their accomplishments.
As we near the end of our second year in the pandemic, we are all feeling drained and many are feeling exhausted. Women and mothers have been especially hard hit. The threat of burnout is very real if we aren’t proactive in caring for ourselves and each other. With that in mind, I have three holiday wishes for each of you: rest, purpose, and revitalization. I hope you each find time to recover from the past year. I hope you create space to engage in personally meaningful activities that you have had to set aside recently. And I hope you find new goals that inspire you clearly and can bring hard-earned wisdom from the past year toward your pursuit of those goals in the New Year.
Speaking of the New Year, the thought of our Annual Meeting in Baltimore (April 6-9, 2022) has buoyed me. We approached record levels of abstract submissions. Our lineup of keynote and master lecturers will provoke us to think about how behavioral medicine can have a greater impact in mitigating and rebuilding from the pandemic, systemic racism, and the climate crisis. We need a healthier and more just world. And our expertise in behavioral medicine can help to create that world if we broaden our perspective in naming and framing the problems we solve.
Taking on the challenge of contributing solutions to complex problems seems a bit audacious on the best of days, let alone during three converging public health tragedies. For that reason, it is critical that each of us take time to recover from the collective and individual trauma we have experienced. With that in mind, I would like to draw your attention to two of our invited speakers in particular. Dr. Jacqueline Kerr, a longtime SBM member, will share her very personal experience with burnout as a working mother and the roadmap she used to revitalize herself. She produces a tremendous podcast, Overcoming Working Mom Burnout, that we can all benefit from. Revitalizing ourselves is only part of the challenge right now. We live in systems and need to revitalize them as well. Building H is a new project that seeks “to build health into everyday life.” Co-founder Steve Downs will share insights from their work to help us all envision ways we can design the healthy and just future we want to revitalize our communities.
As I wrap up this message, we are in the early days of understanding the COVID-19 omicron variant. SBM’s Executive Committee recently adopted a COVID-19 vaccination requirement for the Annual Meeting. Additional countermeasures are described on the conference health and safety FAQ web page. The Executive Committee has a standing call to regularly review a dashboard showing national and Baltimore data on case counts, hospitalizations, and deaths; steps taken by other organizations planning to meet this spring; and much more. We will adjust our plans if needed to keep attendees safe. We are committed to hosting this meeting in person only if we can create an experience that is safe for attendees and their loved ones when they return home. So please get the vaccine or booster if you haven’t already, keep wearing your masks to keep people around you safe in public, test before and after any holiday travel, and quarantine as needed. And in this season of holiday lights, know that the light at the end of this long tunnel is in sight.
Editor's Note: Refocused, Relevant and Resilient
Crystal Y. Lumpkins, PhD; Editor, Outlook

Crystal Y. Lumpkins, PhD
Serving as Outlook Editor has given me an incredible opportunity to serve alongside outstanding SBM leadership and staff. I have learned many lessons and attribute this to observing how this society has responded in uncertain and challenging times. As our President’s Message encourages us to rest, purpose and revitalize during this season, I think about how these holiday wishes for our society provide a moment to pause – we can refocus and remain resilient. This society continues to thrive because of the strategic responsiveness to complex issues in our nation and world, the culture it drives, and commitment to advancing present and future leaders in behavioral medicine. It is no surprise that our society continues to succeed.
In this issue of Outlook, one Past-President shares the work accomplished to address climate change; the Health Policy Council also shares interviews conducted with Health Policy Ambassadors and their work as policy advocates. SBMs Black Past-Presidents also share lessons learned during their presidency and we share a snapshot of SBMs current membership and how the Membership Council will use its report to shape upcoming Council activities. These are just some of the relevant and resourceful articles you will find in this issue.
Finally, I’d like to welcome Dr. Linda Trinh as the incoming Outlook Editor. We are excited that she is on board and is in position to take the reins in spring. I look forward to seeing you in Baltimore in April and wish all of you Happy Holidays.
With Gratitude,
Crystal Y. Lumpkins, PhD
‘Tis the Season for Giving
Marian Fitzgibbon, PhD, Past-President and Development Committee Chair; David Conroy, PhD, President; Margaret Schneider, PhD, President-Elect; and Monica Baskin, PhD, Immediate Past-President

The holiday season has arrived! The season of cold, snow, love, family, and giving. There is no better way to end the year than by giving back to your SBM community and professional home. SBM created the Proven Science—Better Health GIVING Campaign so that we can give back to our members all year long.
Support SBM this holiday season! There are multiple ways to support SBM and we want to help you find the way that works best for you.
Make a Gift Now
Stock Donations
Did you know that stock gifts can give your family a big tax benefit even in a fluctuating market? Stock gifts are the most tax-efficient way for many to give. Appreciated stock gifts receive both a full income tax deduction and eliminate capital gains taxes for those stocks without changing your portfolio.1 Many supporters choose to take advantage of this especially smart way to give.
Make a stock donation this giving season: https://www.sbm.org/UserFiles/SBMStockTransferForm.pdf
Qualified Charitable Distributions (QCDs)
 QCDs or IRA Charitable Rollover Gifts are tax-free gifts transferred directly from your IRA account to SBM. If you’re over 70 ½ years old, making a QCD is a great option to lower your income taxes while doing good for others. QCDs count toward your Required Minimum Distribution (up to $100,000), effectively lower your adjusted gross income and bring about many tax benefits, including eliminating itemized gifts.2
QCDs or IRA Charitable Rollover Gifts are tax-free gifts transferred directly from your IRA account to SBM. If you’re over 70 ½ years old, making a QCD is a great option to lower your income taxes while doing good for others. QCDs count toward your Required Minimum Distribution (up to $100,000), effectively lower your adjusted gross income and bring about many tax benefits, including eliminating itemized gifts.2
To get started on your QCD, contact SBM Development Manager, Eli Rehorst, at erehorst@sbm.org.
Utilize your Donor-Advised Fund
A donor-advised fund account is a simple, tax-savvy investment solution for charitable giving.3 Through your donor-advised fund, you can make a contribution to SBM without paying capital gains taxes.
Corporate Matching Gifts
Did you know that an estimated $4-$7 BILLION in matching gift funds goes unclaimed each year?4 By making a gift to SBM, you can request a matching gift from your employer who will then make their own donation. Over 18 million individuals work for companies with matching gift programs. Maximize your impact by taking advantage of your corporate philanthropy program!
Check to see if your employer matches gifts before making your end of year donation and write in your matched gift here: https://www.sbm.org/UserFiles/SBMDonationPledgeForm.pdf
However you decide to make your end of year gift, just know that we’re so glad you did. From the bottom of our hearts, we thank you and wish you a Happy Holidays!

References
- Freewill 2021 Stock Report: https://www.freewill.com/
- Freewill 2021 QCD Report: https://www.freewill.com/
- Schwab Charitable Donor-Advised Fund: https://www.schwabcharitable.org/donor-advised-funds
- Double the Donation: https://doublethedonation.com/tips/matching-grant-resources/matching-gift-statistics/
Behavioral Medicine and Climate Change: What Can We Do?
Michael A. Diefenbach, PhD✉; SBM Past-President

Climate change is the quintessential and existential challenge of our time. This year, 2021, was, even without the pandemic, a year of superlatives: the hottest year ever recorded, the most wildfires, floods, and hurricanes. In the face of this trend of unabating catastrophes, it is natural to feel anxious, depressed and discouraged about one’s own and one’s family’s future. As behavioral scientists we might even feel that we have little to contribute to the solution to our current problems. We are not engineers, climate scientists, mathematicians, or members of several other fields of perceived relevance to the solution to the climate crisis. But let’s not be defined by what we are not, but what we are and the knowledge we collectively represent! Our unique strength lies in the interdisciplinary nature of the work that we conduct. We work with scientists from the fields of psychology, sociology, epidemiology, anthropology, genetics, and communication science, to name a few; we closely collaborate with members of the health care field (i.e., physicians, nurse, therapists) and we are represented in various industries, such as health care, marketing, and software development. This gives us unprecedented access to the thinking and workings of other fields, as well as an opportunity to assert and disseminate our expertise.
What can each of us do on an individual and professional level to address climate change? I am not urging you to totally change your lifestyle and your habits, although a review of your climate impact might not be a bad idea. I am thinking about your professional impact to address climate change. I am certain that each of our members' expertise can be applied to the climate problem. Whether you are an expert in behavior change theory, a communications and message tailoring expert, whether you are optimizing interventions, or interested in behavioral informatics and technology, your expertise is crucial. Similarly, if you are interested in populations, such as the aged, women or children, or focus on health equity, various aspects of mental health or physical activity, there is need for your involvement in climate research. These are just a few examples that illustrate how we can contribute to climate change research and make a real difference to the future of our society and the planet.
The recent experience with the ongoing COVID-19 pandemic can serve as a blueprint of how crucially important our behavioral expertise has been. It has been pointed out more than once that the solution to the pandemic lies in the execution of simple behaviors: social distancing, mask wearing, hand hygiene, and accepting a lifesaving vaccine. And yet, we have been running into problems communicating evidence effectively, overcoming fear and mistrust, and mounting a coherent response to the pandemic. This situation might not be encouraging when thinking about climate change, but I am convinced that we will learn from our mistakes and develop a more cohesive response to solving climate change. For one, unlike with the COVID-19 pandemic, we have been put on notice, and there is still time to engage, conduct impactful climate-relevant research, and disseminate our expertise. Second, there is no need, and it would be impossible, to do this work alone. There are quite a few sister organizations that are concerned with climate change and have been building task forces and working groups around this issue. SBM as an organization will continue to partner with other organizations to address climate change.
Of all the issues our members listed during the “Provocative Questions” initiative held 2 years ago, climate change and health was the most frequently mentioned topic. Based on this response, my colleague Kara Hall, PhD from the National Cancer Institutes and I chaired a presidential working group that brought together over 30 scientists from wide-ranging fields including experts in air quality, glaciology, health care delivery, cancer and cardiovascular health, communications science, advocacy, and the built environment. The members, both established and early-career scientists, were grouped into five different subgroups, investigating: 1) Climate Change, Behavior, and Health; 2) Health-related Behavior and Climate Change; 3) Health Inequity; 4) Communication; and 5) Policy and Advocacy. Members are finishing up their individual reports, which will be published in a special issue of Translational Behavioral Medicine in the spring of 2022.
I am often approached by members inquiring how they can become more involved in climate change research or advocacy. Here are a few suggestions:
- Realizing that “the time is now.” The conference theme chosen by our current president, David Conroy, PhD, is “The Urgency of Adaptation,” and will focus on, among other things, climate change and health. For the first time in the history of SBM, climate-focused talks and research will be featured and will provide an excellent opportunity to network with other scientists.
- Apply your research expertise to problems related to climate change. The COVID-19 pandemic has shown how quickly our research was able to pivot to pandemic-related themes. The same can be done with climate change. Try to view your research through a climate lens.
- Be attuned to climate-related developments in other contexts and in other organizations that you might belong to. Cross-organization collaborations are needed, and you will be surprised how often our expertise is in demand.
- I am well aware that we are not all born advocates and policymakers, but the communication of our science is crucially important to become more impactful. That is particularly true for climate and health behavior science.
- Advocate for climate-related funding to the NIH and other organizations.
- Submit your climate work to SBM’s Annual Meeting.
Who is SBM? Characterizing our Membership
Claire C. Conley, PhD✉; Loneke Blackman Carr, PhD, RD✉; Scherezade K. Mama, DrPH✉; and Danielle Arigo, PhD✉; SBM Membership Council

SBM is the nation’s premiere multi-disciplinary society promoting rigorous behavioral medicine research and its application to practice and policy. In the past five years, the Membership Council has made an explicit commitment to diversity and inclusion, working to capture multiple dimensions of diversity across our membership, including race, ethnicity, gender identity, sexual orientation, language, culture, religion, mental and physical health, class, education, immigration status, and professional discipline. As a result, we can better understand who SBM members are, and where we need to work to increase diversity.
Below are data on who we are. For this article, we focus on race and ethnicity, gender identity, and discipline. Some of the numbers might surprise you!
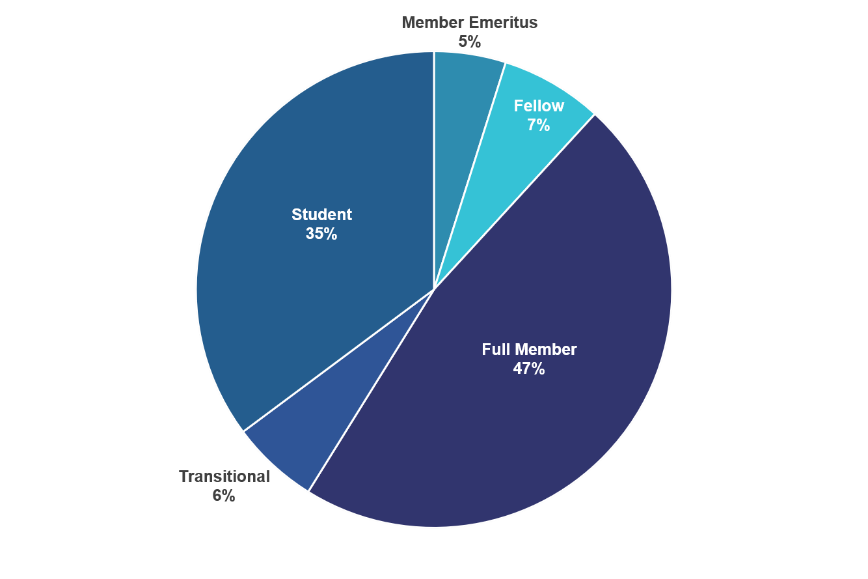
Student members are a critical component of SBM.
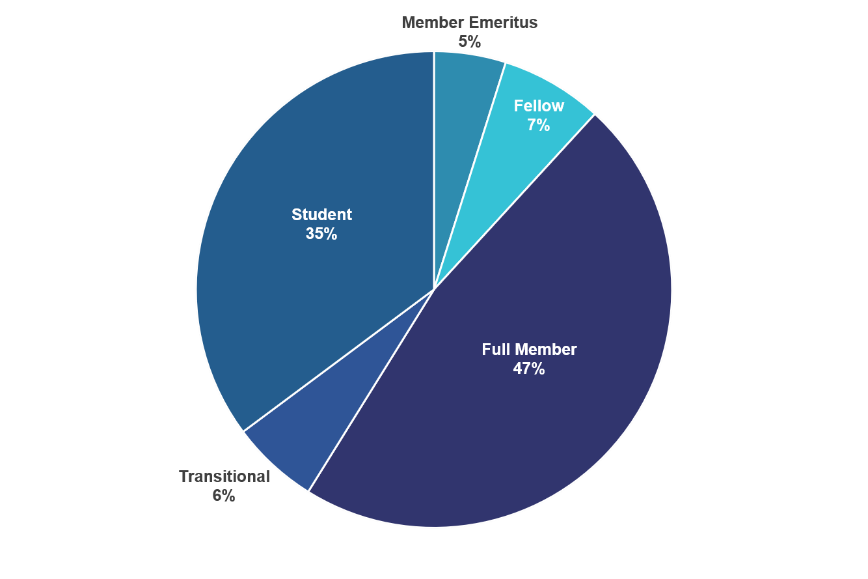
Full Members make up the largest group, and Students come in a close second – nearly 1 in 3 SBM members is a student!
“Transitional Members” are those who have graduated or completed training within the last 2 years. They’re in the process of moving from Student to Full membership. These early-career folks – along with our students – are the future of SBM!
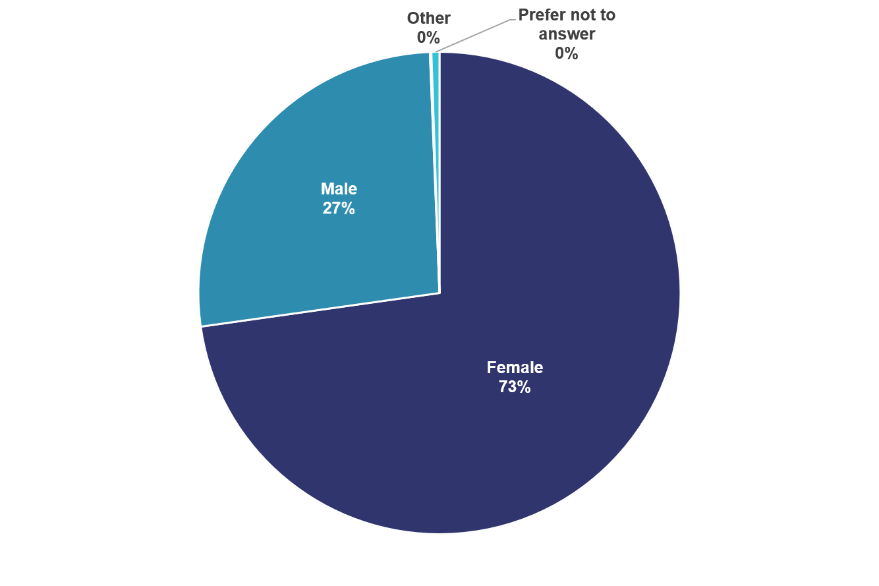
Most SBM members identify as women.
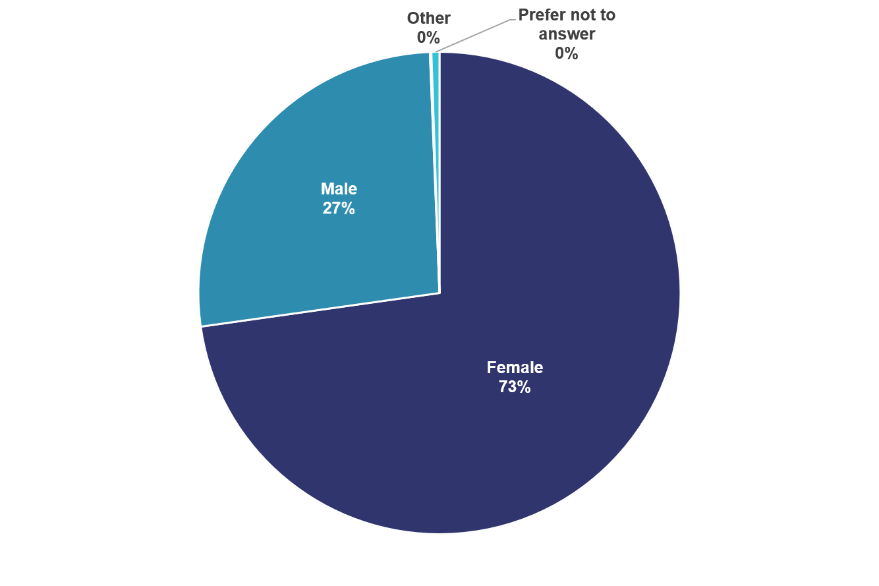
Nearly 3/4 of SBM members identify as women, but this varies by membership type.
Only 35% of Emeritus Members and 50% of Fellows are women. In comparison, women make up 85% of Transitional Members and 80% of Student Members. This may reflect the increasing number of women in the U.S. who are working towards or receiving graduate degrees.
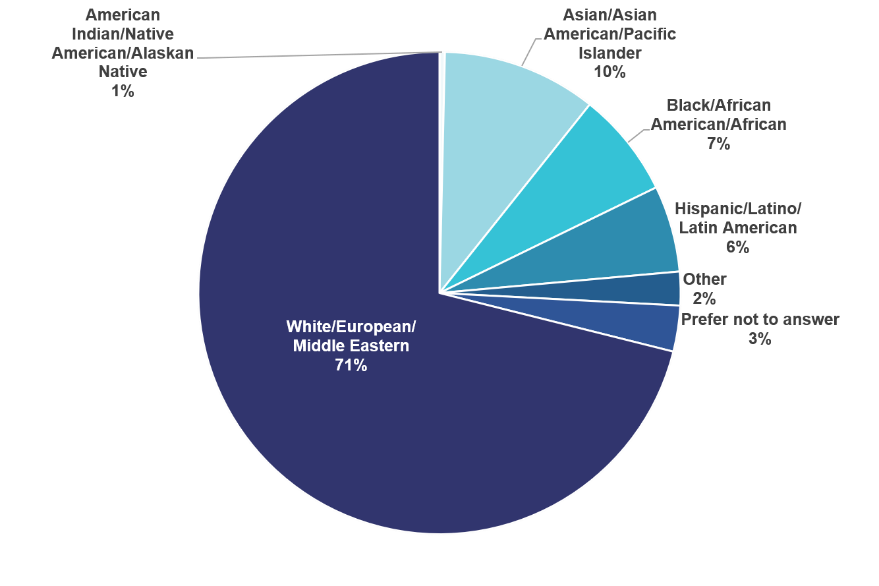
About 14% of SBM members belong to a racial/ethnic group that is historically underrepresented in science.
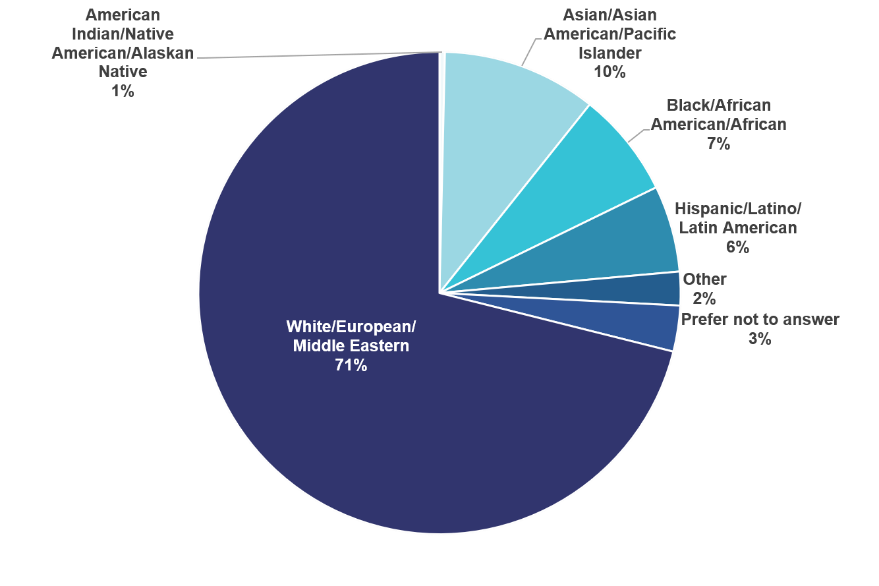
Most SBM members are non-Hispanic White (71%). The next most common racial/ethnic identity is Asian, Asian American, or Pacific Islander (10%).
However, SBM also includes members from groups who have historically been underrepresented in science, including those who identify as Black/African American (7%), Hispanic/Latino (6%), or American Indian or Alaskan Native (1%).
Race and ethnicity of SBM membership also varies by member type. The vast majority of Emeritus Members (98%) and Fellows (92%) are non-Hispanic White. Nearly 20% of Transitional Members and 15% of Student Members identify with a historically underrepresented minority group.
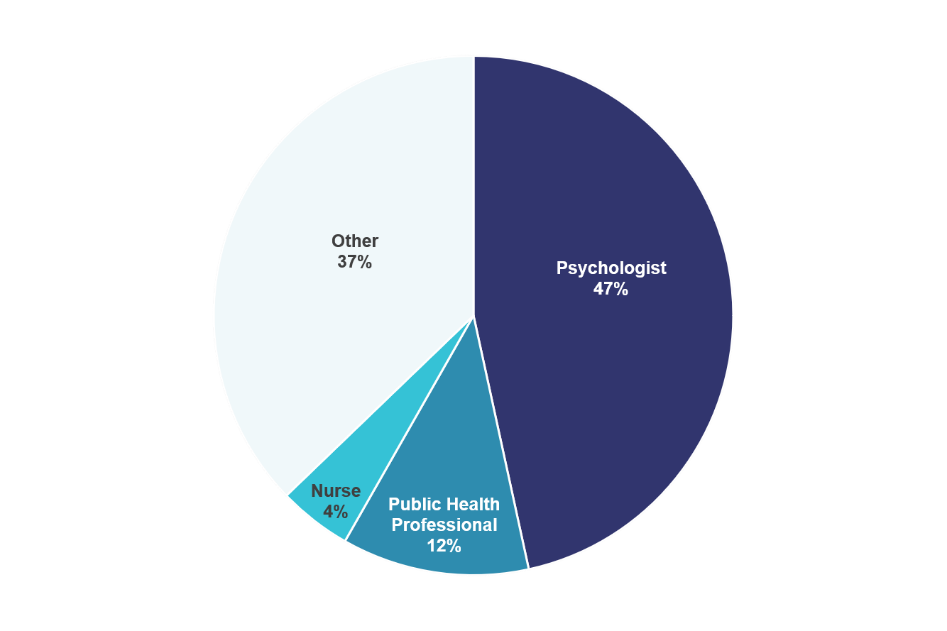
SBM is a multidisciplinary organization.
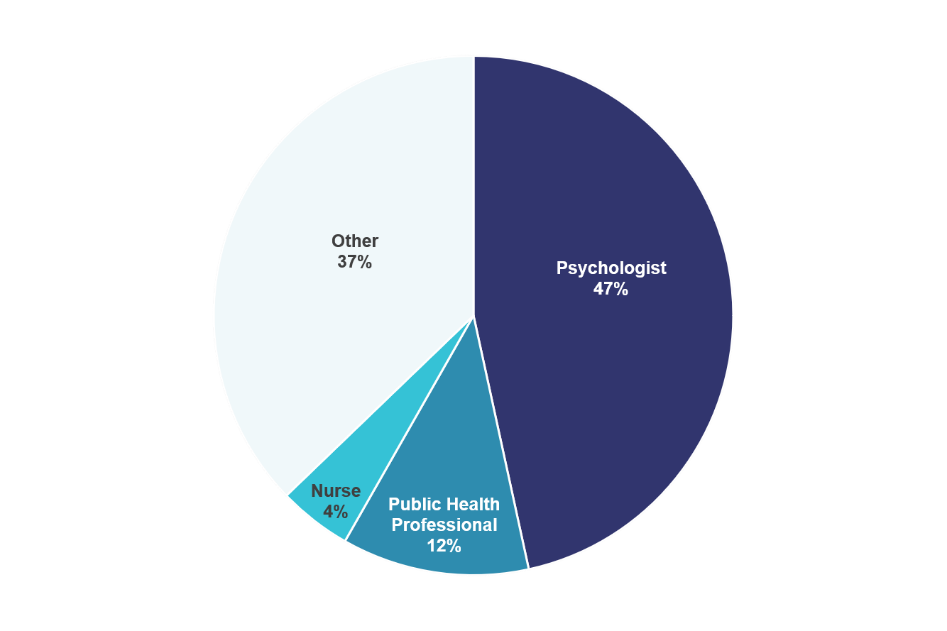
The largest professional groups represented within SBM are psychologists (47%), public health professionals (12%), and nurses (4%). But SBM includes members from over 16 different professional backgrounds!
The “Other” category here includes groups such as epidemiologists, health educators, physicians, dieticians/nutritionists, sociologists, physiologists, social workers, statisticians, anthropologists, pharmacists, geneticists, health economists, and physical therapists.
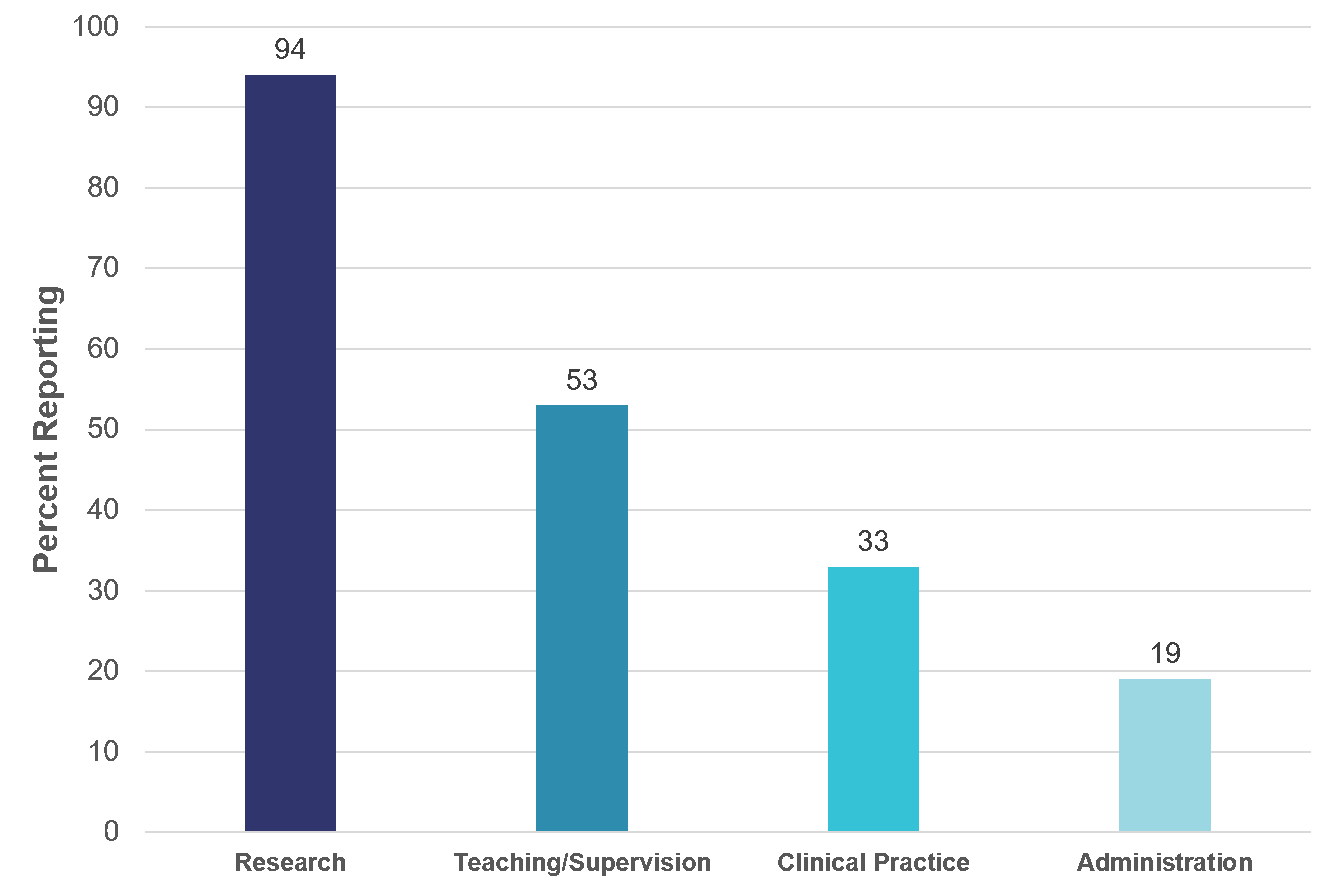
SBM members do more than just research!
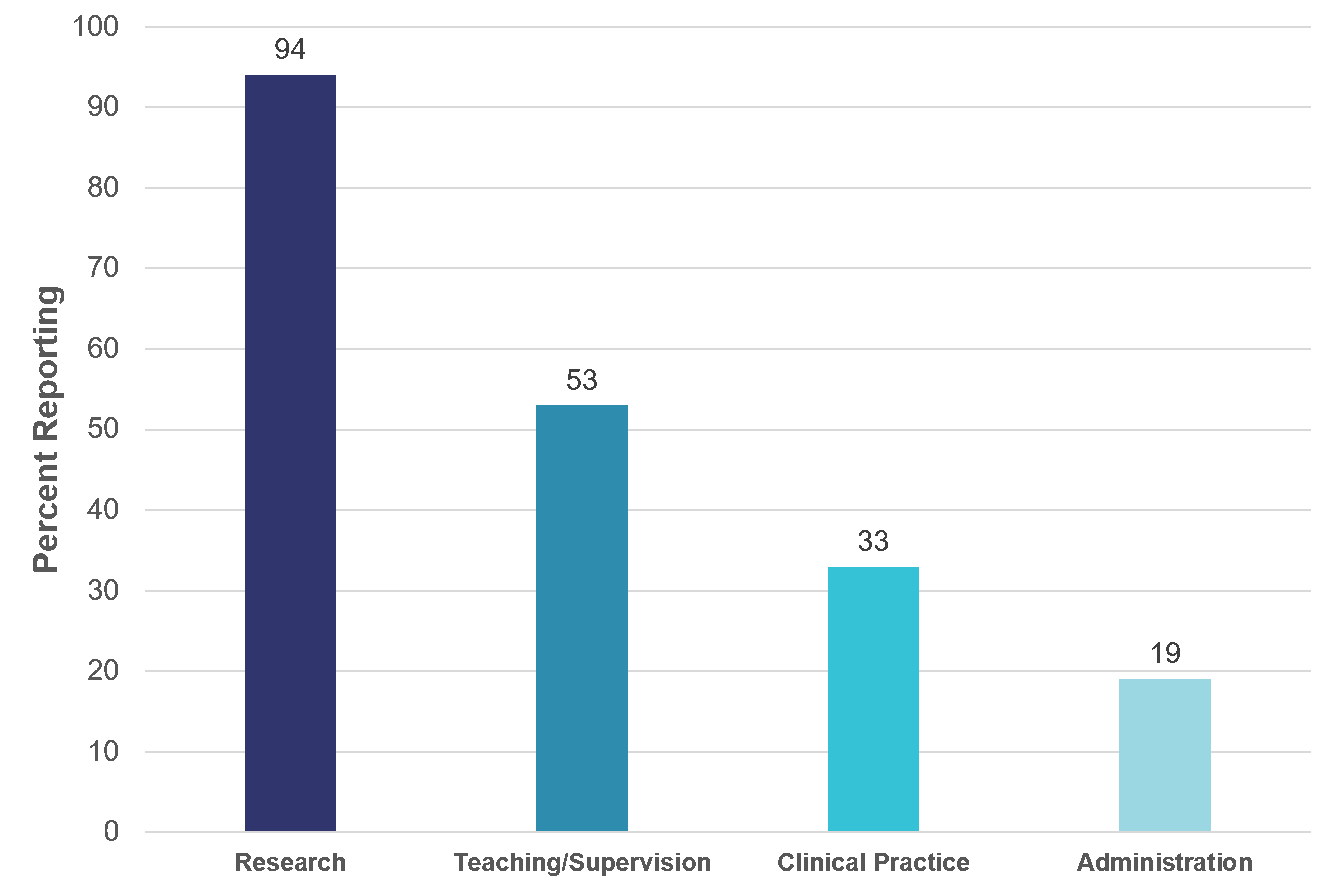
SBM is known for its Annual Meeting and the research presented there, but research is just one part of SBM members’ professional responsibilities.
In addition to research (reported as a professional activity by 94% of members), 53% of members report engaging in teaching or clinical supervision and 33% are actively involved in clinical practice. Although less common, 19% of SBM members also have a role in administration at their institutions.
Moving Forward
As these data demonstrate, SBM is a highly multidisciplinary organization, but we have some work to do to grow our organization. The Membership Council continues to work toward increasing member diversity and monitors these and other indicators.
You can help, too! Spread the word about our multidisciplinary group and the amazing member benefits. Together, we can make SBM a welcoming and inclusive professional home.
Lessons in Diversity, Equity, and Inclusion from SBM's Black Past-Presidents
Stephanie L. Fitzpatrick, PhD✉, SBM Member Delegate


Norman B. Anderson, PhD; Gary G. Bennett, PhD; and Monica L. Baskin, PhD
Given SBM’s commitment to promoting DEI in research, practice, and training, it seems befitting to reflect on how these principles have been fostered over time from the perspective of the three Black Past-Presidents.
Tell us about your leadership trajectory within SBM.
Dr. Anderson: My involvement with SBM really took off as a junior faculty member at Duke, being fortunate to receive the initial New Investigator Award in 1986, and becoming Program Chair in 1988. The highlight of that meeting was calling B.F. Skinner at his Harvard office (he answered the phone) and inviting him to be a keynote speaker, which [he] agreed to do. Unfortunately, he was hospitalized just before the meeting, but nevertheless recorded his keynote address, and gave me an autographed copy of his autobiography from his hospital bed (I still have that book).
Dr. Baskin: My first leadership role in SBM was when President-Elect Dawn Wilson appointed me as Membership Council chair. From there I was elected Member Delegate during which time I was part of the founding steering committee for the SBM Mid-Career Leadership Institute. I later served as the chair of a working group charged by President Gary Bennett to propose recommendations to the board to ensure that DEI was institutionalized in our society. After a short 1-year break from the board, the SBM Nominating Committee encouraged me to run for president and I accepted the charge.
What does DEI mean to you as it pertains to SBM?
Dr. Baskin:
- Inclusion – We must be inclusive in demographics and discipline to allow multiple perspectives to help us achieve our vision of better health for all.
- Equity – We must ensure that all SBM members and initiatives have what they need to succeed. This means that some members and initiatives may require more/less resources than others.
- Diversity – We must embrace, encourage and facilitate a membership that is reflective of our field and the broader society. We must likewise offer diverse resources and platforms to meet the professional needs of our members.
Briefly share your perspectives on the importance of behavioral medicine/science in promoting health equity.
Dr. Bennett: Our experience during the Covid-19 pandemic has shown the critical role of behavioral medicine in health equity. Fundamentally, mitigating disease transmission is a behavioral challenge and in an increasingly interconnected world, it’s critical for us to understand how to best intervene in a wide range of populations and settings. I don’t think there’s a more important priority for our field than preparing to be even more prepared for the next pandemic.
Dr. Anderson: It is fascinating to me that the behavioral medicine perspective on health and illness has become the perspective on addressing health equity, as shown in the focus on the social determinants of health. Our [SBM’s] historical focus on the interaction of socio-cultural, environmental, behavioral, psychological and biological factors in health and illness, and that illnesses can be prevented and treated by focusing on non-biological factors, was really ahead of its time. To me, this perspective is central to any efforts to truly address health equity.
In the 43 year history of SBM, there have been only three Black Presidents and no other BIPOC or Latinx representation. What do you think is needed to enhance the diversity of the SBM leadership pipeline?
Dr. Baskin: To enhance the diversity of the SBM leadership pipeline, we must be more intentional about increasing the diversity of our membership, better educate the full membership about why diversity in leadership is important, increase awareness by under-represented groups of leadership opportunities in SBM, sponsor BIPOC members, and continuously evaluate and address systemic barriers to greater diversity.
What words of wisdom do you have for behavioral scientists and practitioners from underrepresented backgrounds?
Dr. Bennett: Mentoring and advocacy are both critical to your career success. You need both, and they’re unlikely to be found in the same person. Distractions are myriad for all of us, and especially so for underrepresented scientists. Find ways to ignore the flood of requests and focus on creating the best science you can. At the end of the day, improving the health of people and populations, and career success derive most proximally from scholarly excellence.
Dr. Baskin:
- Get involved (and don’t just wait for someone to ask you)
- Get a group of peers that you can always count on for support
- Identify potential sponsors and reach out to them (and it's OK if it takes more than one attempt)
What successes has SBM had related to DEI?
Dr. Anderson: SBM was really the first organization that validated and affirmed my early research on hypertension in African Americans, at a time when research on “minority groups” was nearly non-existent in health sciences circles and clearly under-valued. I even had one white senior colleague warn me that “no one gets well-known by studying one group,” failing to recognize that most behavioral research at the time was conducted on one group--whites. But I found a receptive home at SBM. It is great to see that SBM has become a really strong place where issues of health equity are so prominent in presentations.
Dr. Baskin: There have been several successes including:
- Procured more complete member data records to better track diversity
- Promoted leadership diversity in SBM elections, fellows and award recipients, councils and committees with criteria for nominations/selections reflecting values related to DEI
- Diversified and strengthened SBM’s early-career leaders via pre-conference training and mentoring opportunities.
- Adopted a policy that institutionalizes SBM’s commitment to diversity in its leadership, membership, programs, activities and decision making
Small Doses, Large Hesitancy: Addressing Parent Hesitancy Against Vaccinating Children for COVID-19
Christina Cordero, PhD✉; Shu-Fang Shih, PhD, MSc, MBA✉; Marissa Kobayashi, PhD✉; and Sherecce Fields, PhD✉; Child and Family Health SIG

Children ages 5 to 11 years can now receive vaccines to protect them from COVID-19. In early November, the Food and Drug Administration authorized emergency use of the Pfizer BioNTech COVID-19 vaccine followed by a recommendation from the Centers for Disease Control and Prevention (CDC). Data from ongoing clinical trials on children aged 5 to 11 years showed that a lower dose of the vaccine was 90.7% effective in preventing symptomatic COVID-19 infection and no serious adverse events were reported.1 Despite the data on the safety and high effectiveness of the vaccine, many parents continue to express hesitancy and reluctance. According to an October survey, 27% of parents of 5-11year-olds reported that they will get their children vaccinated right away, 33% said they will wait a while, and 30% said their child will definitely not get the vaccine.2 This last category has been increasing from previous iterations of the survey.2 Parents’ biggest concerns were long-term side effects (76%), serious side effects (71%), and negative impact on future fertility (66%).2 Concerns about fertility have no basis in science3 and have become widespread through social media misinformation. Parents’ political identification and educational attainment also predict their readiness to vaccinate their children.4
To protect children from COVID-19, the Biden Administration proposed a plan with the following goals: to secure vaccine supply, to support education and engagement efforts to build public trust, and, perhaps most importantly, to make vaccinations free and easily accessible.5 The U.S. Department of Health and Human Services will conduct a national public education campaign to reach parents and guardians with accurate and culturally responsive information about the vaccine and the risks that COVID-19 poses to children. Since pediatricians and other health care providers will likely be the main trusted resource for parents, the CDC provides health education materials to those practitioners and the CDC website provides a link to start the process to become a vaccination provider.6 However, presenting health education material may not be enough for parents to make the decision to vaccinate. In fact, recent studies show that pro-vaccine communications are often ineffective and may backfire, decreasing intentions to vaccinate, particularly among those who are already hesitant.7-9
Understanding how people make decisions regarding vaccination will provide insights for designing messages to promote vaccine acceptance. There are many factors that influence vaccine decision-making, including individual risk perception, personal beliefs, underlying moral values, attitudes, and personal barriers and motivators, as well as socio-psychological drivers and cultural norms and traditions.10,11 Vaccine promotion messages should be evidence-based, culturally appropriate, and designed specifically for the social and behavioral context. The World Health Organization proposes that vaccine hesitancy is best addressed by building trust and relationships, listening to and understanding people, and communicating risk and shaping messages to the appropriate audience.12 While scientific evidence supports vaccination, studies suggest that statistics and facts may not be effective at communicating disease risk to a general population. Research shows that the probability of health effects from vaccines or disease is not as important to parents’ vaccine decision-making as the impact of disease severity or vaccine side effects.13 Instead, narrative-based messages highlighting disease severity may be more effective than statistical facts.14
Compared with other respiratory diseases such as influenza, children still face a high risk of mortality due to COVID-19.15 In fact, COVID-19 has emerged as a Top 10 leading cause of death among children in the US16 although the risk for severe COVID-19 disease is lower in children than adults. Vaccinating children appears to be the key to preventing future waves of COVID-19 in the United States17 and is also an important way to protect higher-risk family members and people in the community. High vaccination rates in children can also signal a return to normal for children who have especially felt the psychological, social, developmental, and educational impact of the pandemic.
References
- The United States Food and Drug Administration. (2021, October 29). FDA Authorizes Pfizer-BioNTech COVID-19 Vaccine for Emergency Use in Children 5 through 11 Years of Age. https://www.fda.gov/news-events/press-announcements/fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use-children-5-through-11-years-age
- The Kaiser Family Foundation. (2021, October 28). KFF COVID-19 Vaccine Monitor: October 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-october-2021/
- Centers for Disease Control and Prevention. (2021, November 4). COVID-19 Vaccines for Children and Teens. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/children-teens.html
- Gallup. (2021, October 29). Parents' Vaccination Intentions for Young Children Steady. news.gallup.com/poll/356774/parents-vaccination-intentions-young-children-steady.aspx
- The White House. (2021, October 20). FACT SHEET: Biden Administration Announces Update on Operational Planning for COVID-19 Vaccinations for Kids Ages 5-11. https://www.whitehouse.gov/briefing-room/statements-releases/2021/10/20/fact-sheet-biden-administration-announces-update-on-operational-planning-for-covid-19-vaccinations-for-kids-ages-5-11/
- Centers for Disease Control and Prevention. (2021, November 16). How to Talk with Parents and Caregivers about COVID-19 Vaccination: Tips for Pediatricians, Family Medicine Practitioners, Nurses, Pharmacists, Public Health Officials, & Other Vaccine Providers. https://www.cdc.gov/vaccines/covid-19/hcp/pediatrician.html
- Nyhan B, Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33(3):459-464.
- Pluviano S, Watt C, Della Sala S. Misinformation lingers in memory: Failure of three pro-vaccination strategies. PLoS One. 2017;12(7):e0181640.
- Pluviano S, Watt C, Ragazzini G, Della Sala S. Parents’ beliefs in misinformation about vaccines are strengthened by pro-vaccine campaigns. Cogn Process. 2019;20(3):325-331.
- Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. 2015;2(1):61–73. doi:10.1177/2372732215600716
- UNICEF Demand for Immunization Team and Yale Institute of Global Health. (2020, December). Vaccine Messaging Guide. https://www.unicef.org/media/93661/file/Vaccine&hx0025;20messaging&hx0025;20guide.pdf
- World Health Organization Regional Office for Europe. (2017). Vaccination and Trust: How concerns arise and the role of communication in mitigating crises. https://www.euro.who.int/__data/assets/pdf_file/0004/329647/Vaccines-and-trust.PDF
- Sadique MZ, Devlin N, Edmunds WJ, Parkin D. The effect of perceived risks on the demand for vaccination: results from a discrete choice experiment. PLoS One. 2013;8(2):e54149
- Finnegan G, Holt D, English PM, Glismann S, Thomson A, Salisbury DM, Bogaerts H, Bonanni P. Lessons from an online vaccine communication project. Vaccine. 2018 Jun 16. pii: S0264-410X(18)30612-1.
- Piroth, L., Cottenet, J., Mariet, A. S., Bonniaud, P., Blot, M., Tubert-Bitter, P., & Quantin, C. (2021). Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. The Lancet Respiratory Medicine, 9(3), 251-259.https://doi.org/10.1016/j.vaccine.2021.08.005
- Centers for Disease Control and Prevention. (2021). Underlying Cause of Death, 1999-2019. CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) Search. https://wonder.cdc.gov/ucd-icd10.html
- Schleiss, M. R., John, C. C., & Permar, S. R. (2021). Children are the key to the Endgame: A case for routine pediatric COVID vaccination. Vaccine, 39(38), 5333–5336.
I Know the Vaccine is Important but How Do I Talk to My Patients about It? Evidence-Based Ways to Encourage COVID Vaccines and Masking
Jocelyn E. Remmert, PhD✉ and Jennifer S. Funderburk, PhD✉; Integrated Primary Care SIG

Now that the COVID-19 vaccine has become more widely available, healthcare professionals such as primary care providers and teams will be at the forefront of encouraging and talking to reluctant patients about it. Due to the highly politicized nature of COVID-19, these conversations can be difficult. That’s why we’ve worked with expert behavioral researchers in communication, behavioral medicine, decision making, and health equity to put together a few key tips to use in your regular clinical practice.
First and foremost, we encourage you to take five minutes to have those conversations with patients. It is tempting to avoid these conversations due to the sensitive nature of the topic, but research shows that healthcare providers are trusted individuals to patients and your voice matters more than you likely think it does.1
Some important evidence-based communication tips based on other research include:
- Start by talking to patients about the vaccine like you would any other, if it's discussed as a part of regular medical care, many patients will agree without additional discussion: “When would you like to schedule your COVID-19 vaccine?”
- If you’re short on time (and who isn’t these days?), choose to spend the time you do have discussing the vaccine with community leaders (e.g., pastors, police officers, teachers), as they can influence their larger community.2,3
- If there are hesitancies or skepticism, LISTEN. It may be frustrating, but the most important piece of communication is making the patient feel understood.4
- If the person doesn’t understand why masking in large public areas and the vaccine is needed, consider using a metaphor of slices of Swiss cheese stacked. “Each slice of cheese is one layer of protection, like wearing a mask, but each slice has holes. If you stack them, you get the best protection.”
Some example statements you can use in different situations:
- If a patient shares misinformation, ask permission and be non-judgmental:
- “Is it OK if I share some additional information about how I understand the evidence to help you make your decision? It’s important to me to that my patients have all the information they need to make the right decision for them.”
- If your patient is anxious or skeptical, provide your opinion while acknowledging it is the patient’s decision:
- “I was also worried about this new COVID-19 vaccine/shot, so I read about what the doctors have done. While it’s a new vaccine/shot, it went through the same hoops as other medications I give you, and I can assure you it is safe and it works. I have seen people with COVID-19, and believe me, it is not something you want. My job is to help you stay healthy. Like other medications I give you, I believe this vaccine/shot is important for your health. However, the decision is up to you.”
Need more ideas? Want to share with your coworkers? Our resource has even more statements and handouts to share with patients. Let’s all work together to help our communities heal from COVID-19.
References
- Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000;15(7):509-513. doi:10.1046/j.1525-1497.2000.11002.x
- Liljas AEM, Walters K, Jovicic A, et al. Strategies to improve engagement of “hard to reach” older people in research on health promotion: a systematic review. BMC Public Health. 2017;17(1):349. doi:10.1186/s12889-017-4241-8
- Winkfield KM, Regnante JM, Miller-Sonet E, González ET, Freund KM, Doykos PM. Development of an Actionable Framework to Address Cancer Care Disparities in Medically Underserved Populations in the United States: Expert Roundtable Recommendations. JCO Oncology Practice. 2021;17(3):e278-e293. doi:10.1200/OP.20.00630
- Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. 2017;139(1):e20161764. doi:10.1542/peds.2016-176
“Quite a Change from Academia” – Words of Wisdom from a Clinical Psychologist in Industry
Jessee Dietch, PhD✉; Eric Zhou, PhD✉; and Michael Mead, PhD✉; Sleep SIG

Jason Ong, PhD
The explosion of health-focused companies, particularly those that leverage technology, has led to increasing opportunities for clinical psychologists to apply their training in a fast-paced business setting. Yet many clinical psychologists have little access to information about these “alternate” career paths that are steadily becoming more mainstream.
As part of the Sleep Special Interest Group Outlook article series on alternative career paths in clinical psychology, we had the joy of connecting with Dr. Jason Ong to learn more about careers in industry. Dr. Ong is a clinical psychologist who recently made a career change as a highly successful researcher and clinician at an academic medical center to an exciting new position with Nox Health. Here, Dr. Ong shares his experiences including what motivated the career change and advice for anyone considering a similar path.
Please describe your role in industry.
I am the Director of the Behavioral Sleep Medicine (BSM) program at Nox Health. My primary role is to develop a BSM service that integrates technology and care providers as part of a sleep healthcare system at Nox Health.
As a highly successful academic, what pushed you to consider moving to industry?
I have always been interested in business and entrepreneurship. When this opportunity came up, I wanted to see if I could take the things I have learned in my research and clinical work and merge them with my interest in business and entrepreneurship. I was also getting increasingly frustrated at how slow things move in academic research.
What are the differences in terms of your responsibilities and day-to-day work in industry, compared to academia?
I think the main difference is that I get to work together in multidisciplinary teams that now include business leaders, tech developers, operational managers, and clinical folks. This is quite a change from academia, where you are primarily responsible for yourself (and your lab as an extension of yourself) and if you work in a multidisciplinary setting, it usually means different medical specialties or nurses and physicians. Also, my role now focuses more on strategic development rather than seeing patients or writing grants or manuscripts. It’s similar to moving from a coach or player, where the focus is on winning games, to a front-office position, where the focus is on building a championship team, managing the salary cap, and selling tickets.
For some, an appeal of working in academics is the flexibility of the work schedule and the type of work you pursue. Has there been an adjustment to your role in industry?
My position is a remote-work position that does not involve direct patient care at this time, so I would say that I have even more flexibility than I had in my academic position. People in our company are very respectful of work/life balance so I rarely get emails after hours and there are no expectations to work after hours or on the weekends. If there has been any adjustment, it’s that I get to spend more time with my family and my quality of life has improved!
What is something about working in industry that you wished you had known before you took your position?
One myth that I think is often perpetuated in academic circles is that the smart people are in academia and the greedy people are in industry (or all they want to do is make money). But I was speaking to a colleague who also recently left a successful academic career for an industry position and we were both talking about how impressive the intellectual resources were in our respective companies. Maybe it doesn’t generalize to other companies, but I think it’s a myth perpetuated by academicians designed to keep people in academia!
What are drawbacks to or considerations for working in industry? What are the greatest benefits?
Things move quickly in industry and job security is not the same as academia, especially if you are tenured. So, it can be a high-risk venture and you need to be prepared for that. However, the reward can be very high, especially financially, if you work for a start-up company. I think learning business fundamentals is also a helpful skill that generalizes across sectors.
For someone who is curious about exploring an industry-based job, what advice would you give them as they start their search?
I would highly encourage anyone considering a move to industry to first talk to others – mentors, colleagues, those who have made the change – and get their input. When considering an industry job, you might also need to ask questions about the financial aspects of the company, especially if it is a start-up company. We don’t need to do that in academia, so you might need to learn a bit about how to evaluate a company’s financial situation. Finally, consider your skillset (e.g., do you like writing and managing grants? Seeing patients?), tolerance for risk, and whether or not you like to work in teams or do your own thing.
For junior faculty or those out of training, it might be more difficult to go back to academia if things don’t work out so you probably want to choose more carefully. For established faculty, the risk/reward and work/life balance will probably be important considerations.
Is there anything you miss about academia? Anything you don’t miss at all?
I miss seeing my friends and colleagues on a day-to-day basis and the opportunity to talk about really cool and interesting research ideas. But I have an adjunct appointment at Northwestern, so I am still involved in mentoring and collaborating on research projects.
I absolutely do not miss the nitpicking and the incessant need to critique that is commonplace in academia, especially with grants and manuscripts. I was part of this system so I am guilty of it as well. But it has been very refreshing to focus on the big picture and what is most important rather than constantly responding to a bunch of critiques, which can derail or delay projects. I also do not miss RVUs or being on soft money.
Is there anything else you would like to share?
I am happy to talk to anyone who has questions about working in industry or is considering a change from academia to industry.
Dr. Ong can be reached at jong@noxhealth.com
Translating Research to Policy: A Q&A with SBM's Health Policy Ambassadors
Joanna Buscemi, PhD✉; Health Policy Council Chair

Our Health Policy Ambassadors strive to close research to policy translation gaps through regular contact and relationship building with legislative staff. Our key priority areas aim to educate lawmakers about 1) evidence-based ways to ensure children from all income levels have access to healthy foods; 2) evidence-based ways to best manage pain and combat opioid misuse; and 3) the unique healthcare needs of rural populations and evidence-based strategies to improve their health outcomes and quality of life. There are currently 28 Ambassadors building relationships with legislative staff across the country. We spoke with Heather Hardin, PhD; Hallie Espel-Huynh, PhD; Betsy Seng, PhD; Dori Pekmezi, PhD; and Thelma Mielenz, PhD about challenges and successes in the Health Policy Ambassador program and the skills they have built as policy advocates.
For those not familiar with the Health Policy Ambassador Program, how would you describe its purpose and function?
Dr. Hardin: The purpose of the Health Policy Ambassador program is to get evidence-based health information to legislators who have the power to influence national health policy. This is done by building a relationship with the legislator’s health policy staff, finding out what is important to the legislator, and sharing my expertise with them.
Dr. Espel-Huynh: Our purpose is to serve as a reliable and informative resource to policymakers, specifically focusing on topics that are under our area of expertise in behavioral medicine. The goal is to help policymakers support, prioritize, and craft legislation that is informed by empirical evidence and prioritizes the needs of our patients.
Dr. Seng: The purpose is to use the science of behavioral medicine to inform national decision-makers as they grapple with how to best address public health challenges.
What are the most challenging parts of building relationships with legislative staffers?
Dr. Pekmezi: Legislative staffers have busy schedules, which can change on a dime and make building relationships challenging.
Dr. Espel-Huynh: The most challenging part for me has been learning the language of policy-making. Scientists and practitioners have certain priorities that are driven by population needs and funding priorities. Policymakers often have complementary interests, but they might have different policy-focused motivations for focusing on them. Learning how to speak about behavioral medicine in a way that is plain, simple, and compelling to policymakers has been the biggest challenge for me, and one I'm still learning.
What do you think has been the most meaningful outcome of your conversations with policymakers/staff?
Dr. Hardin: The most meaningful outcome of my conversations with the legislative staffer occurred early on in my relationship with them. The legislative staffer asked for some evidence about telehealth, which I found and shared with them. However, they did not seem receptive to my recommendation, and I felt a bit disappointed. A month or so later, the legislator’s e-newsletter described a new telehealth bill they had introduced, and it included my recommendation. It was satisfying to see my efforts pay off.
Dr. Seng: I really don't think the staffers I have spoken with knew how much science already exists to inform policy. The idea that there is a whole field of people who study behavioral issues in public health was new to them. I think they definitely see us as a resource.
Why should other members become an Ambassador?
Dr. Mielenz: It is a rich learning experience to see that our published work can make a real difference.
Dr. Hardin: SBM members have a wealth of expertise to share with others—the Health Policy Ambassador program is a way to influence the implementation of evidence-based recommendations into national policy, which can influence practice and people on a grand scale.
Dr. Pekmezi: Becoming an ambassador provides the opportunity to learn more the health policy process, practice science communication and meet/interact with the people who are in “the room where it happens."
Dr. Seng: It is gratifying to build these relationships and see your work being translated in the policy arena.
What skills have you learned as an Ambassador that have improved other areas of your career?
Dr. Hardin: The Health Policy Ambassador program has helped me to think about the big picture of rural health, how my work fits in, and my role in making positive changes in health care.
Dr. Espel-Huynh: I have learned so much about the policies that support (or get in the way of) nutrition and healthy lifestyle behaviors at the population level--for more than I'd ever learn in doing research alone. The work I do as an Ambassador helps me to think big-picture about the research questions I'm asking, particularly how the results will fit into the broader context of our legislative and policy environment.
Is Your Health Research Going Digital? Check Out These Tools and Resources to Guide Ethical Practices
Camille Nebeker, EdD, MS✉; Rebecca Bartlett Ellis, PhD✉; Megan Oser, PhD✉; and Stephanie Goldstein, PhD✉; SBM Digital Health Council

The Digital Health Council is excited to announce a new ethics subcommittee that will assist SBM members in considering the Ethical, Legal and Social Implications (aka ELSIs) of digital health. Digital health is an umbrella term that is used to describe technology-based strategies and tools that are used in health research and healthcare. For example, if you use social media platforms, remote/wearable sensors, computational informatics, virtual/augmented reality, artificial intelligence, smartphone apps for data capture or to deliver an intervention you are in digital health!
Our Digital Health Ethics committee includes Drs. Camille Nebeker, Associate Professor at UC San Diego and Director or ReCODE Health; Stephanie Goldstein, Assistant Professor (Research) at Brown University; Megan Oser, Digital Health Strategist and Rebecca Bartlett Ellis, Associate Professor at Indiana University. Our group is working to help SBM and its members by: assisting researchers of all backgrounds and career levels with ethically incorporating digital health into their work; curating and managing resources to support the ethical design and conduct of studies that use digital health tools for assessment and/or intervention; championing partnerships with initiatives that will benefit members; liaising with other SBM committees to ensure ELSI is a cross-cutting priority within and across SBM; and working to highlight ELSI-related training and content at the annual meeting.
One of our first steps is to conduct a Digital Health Needs Assessment. Help us by completing this survey – only one month left! We plan to share results via an SBM Webinar in 2022 – more on that soon!
What’s available to SBM members right now…
We’re excited to share that the SBM Board approved a proposal to partner with ReCODE Health [Research Center for Optimal Digital Ethics in Health] https://recode.health. ReCODE Health is a research center at UC San Diego that provides consultation and education to guide the design and conduct of digital health research. In addition, the ReCODE Health team conducts research to guide digital health policy and practices. This new partnership means that SBM members will have access to the Digital Health Checklist and Framework that was developed by SBM-affiliated behavioral scientists who had expressed a need for guidance as they designed their studies. The checklist can be accessed via the ReCODE Health website and can be used to help make decisions about selecting technologies for use in research.
Coming soon, the ReCODE Health team has redesigned its Resource Library. Soon you will be able to search the Resource Library to find approved research protocols and consent language to help kick start your digital health research planning. In addition, you will have access to a global network of digital health researchers, technologists, and experts in ethical and social aspects of digital health. This ReCODE Health Forum is where you can seek input on your digital health research design or provide solutions for someone in need.
Insights from Obesity and Eating Disorders Researchers on Diversity, Equity, and Inclusion
Christine Jovanovic, PhD, MPH✉; Anne Claire Grammer, MA✉; Jackie Hayes, PhD✉; and Jennifer Mandelbaum, MPH✉; Obesity and Eating Disorders SIG



Kristin Heron, PhD; Roger Figueroa, PhD, MPH; and Tiffany Carson, PhD, MPH
The Obesity and Eating Disorders (OED) Special Interest Group interviewed Kristin Heron, Associate Professor at Old Dominion University; Roger Figueroa, Assistant Professor at Cornell University; and Tiffany Carson, Associate Member of the H. Lee Moffitt Cancer Center and Research Institute, about their perspectives on Diversity, Equity, and Inclusion (DEI) in OED research. With increased emphasis on the social determinants of health and health equity, these experts’ insight on integrating DEI across OED research will be of interest to a broad range of researchers at SBM. We present selections from interviews with these experts.
A lot of work is prioritizing DEI in eating and weight management research and programming. What do you find most exciting?
Dr. Carson: Efforts to understand and address the role of systemic racism and other race-associated societal factors in eating and weight management. I am excited that researchers are recognizing that race and/or ethnicity are not just variables to control for statistically.
Dr. Heron: The ways in which we are expanding our understanding of diversity to include a wider range of aspects of people’s identities – race, ethnicity, gender, sexual orientation, age, religion, ability, language, socioeconomic status, geographic setting, etc. – is really exciting.
Dr. Figueroa: The sense of urgency to account for the lived experiences of those who have been historically excluded and marginalized in eating and weight management research.
What are the biggest research gaps in this area?
Dr. Heron: Recognizing the importance of considering intersectionality, or how being a member of multiple marginalized groups may impact health.
Dr. Figueroa: Eating and weight management research has predominantly focused on individual and/or social behavior change. We need more attention on upstream factors (i.e., institutionalized racism, economic inequality, residential segregation) shaping the context for social and behavioral outcomes.
Dr. Carson: The dissemination and implementation of evidence-based guidelines to diverse communities with long-term sustainability. Finding ways to educate and empower individuals from all backgrounds to leverage findings from research to improve their health.
What would you consider you biggest "lessons learned" or pitfalls to avoid?
Dr. Figueroa: We need to include and support hardly-reached populations, as well as address the underrepresentation and lack of (financial, logistical, psychological, social) support of minoritized scientists.
Dr. Heron: Finding community partners early in the project planning process is so important for the success of this work.
Dr. Carson: Understanding that things may not always happen as quickly as I would hope. Background work must be done to understand and set priorities that interest all stakeholders.
What advice would you offer trainees starting in DEI in eating and weight management research?
Dr. Heron: Find collaborators or mentors with expertise in DEI, even if their content interests are outside your own.
Dr. Figueroa: Seek well-rounded and rigorous training that provides an understanding and tools to account for upstream social and structural factors.
Dr. Carson: Understand this work often requires relationship building, data collection, and the courage to challenge practices and systems that have been in place for a long time.
Looking Within: Can Studies of Intra-Individual Variability Improve Multiple Health Behavior Change Interventions?
Tyler Mason, PhD✉ and Tammy Stump, PhD✉; Multiple Health Behavior Change and Multi-Morbidities (MHBCM) SIG

Several decades of health behavior research have provided numerous insights into the factors that contribute to successful behavior change, including attitudes, self-efficacy, and perceived risks. For many health behaviors, though, a focus on individual-level differences is just the tip of the iceberg when it comes to understanding what predicts behavior and how best to intervene. Lifestyle behaviors, such as physical activity, eating a healthy diet, using sun protection, and smoking, must be performed, or avoided, consistently over time to improve health outcomes.1 Such behaviors are dynamic and multiply-determined; they vary based on intra-individual variables, including the individual’s momentary physical and social environments, affect, and cognition. New insights on these intra-individual dynamics may provide a fresh perspective to ongoing questions within the area of multiple health behavior change, including which behaviors should be combined within the same intervention and whether to intervene on multiple behaviors simultaneously or sequentially.
Methodological advances (e.g., passive sensing, ecological momentary assessment) and statistical innovations (e.g., mixed-effects location-scale modeling) permit rigorous evaluation of the micro-temporal dynamics of lifestyle behaviors.2 As a few examples: We now have direct evidence that periods of stress or negative affect have an immediate impact on smoking and that individuals who experience the most consistent relationship between smoking and decreases in negative affect have the highest levels of smoking.3 For physical activity, children’s higher-than-usual positive affect not only promotes their own physical activity but also that of their mother.4 For healthy eating, unplanned meals, experiencing negative emotions (boredom, stress), and time of day (evening) predict dietary lapses.5
Less explored by these micro-temporal evaluations is the dynamic interplay between various health behaviors. Linkages among health behaviors can be synergistic (e.g., eating a healthier diet can lead to healthy decreases in sedentary behavior)6 or antagonistic (e.g., those who are more physically active have a higher prevalence of sunburn).7 A focus on intra-individual variation can provide new insights explaining the associations among various health behaviors. For instance, these methods would allow us to learn more about the specific contexts in which health behaviors tend to co-occur and about potential pathways that operate on an intra-individual level, such as a change in affect or other physical state arising through the performance of one behavior having downstream consequences for other behaviors.
With most common health conditions – including cardiovascular disease and cancer – being impacted by multiple behavioral factors, behavioral scientists can make the biggest impact by using approaches that target change in multiple behaviors. Studies of intra-individual variability hold promise for informing refinements to these approaches along with applications of advanced intervention methods (e.g., just-in-time adaptive interventions, continuous tuning interventions) that maximize change to multiple behaviors.8
References
- Dunton, G. F. (2018). Sustaining health-protective behaviors such as physical activity and healthy eating. JAMA, 320(7), 639-640.
- Dunton, G. F., Rothman, A. J., Leventhal, A. M., & Intille, S. S. (2021). How intensive longitudinal data can stimulate advances in health behavior maintenance theories and interventions. Translational behavioral medicine, 11(1), 281-286.
- Hedeker, D., Mermelstein, R. J., & Demirtas, H. (2012). Modeling between‐subject and within‐subject variances in ecological momentary assessment data using mixed‐effects location scale models. Statistics in Medicine, 31(27), 3328-3336.
- Yang, C. H., Huh, J., Mason, T. B., Belcher, B. R., Kanning, M., & Dunton, G. F. (2020). Mother-child dyadic influences of affect on everyday movement behaviors: evidence from an ecological momentary assessment study. International Journal of Behavioral Nutrition and Physical Activity, 17, 1-11.
- Goldstein, S. P., Dochat, C., Schumacher, L. M., Manasse, S. M., Crosby, R. D., Thomas, J. G., ... & Forman, E. M. (2018). Using ecological momentary assessment to better understand dietary lapse types. Appetite, 129, 198-206.
- Spring, B., Schneider, K., McFadden, H. G., Vaughn, J., Kozak, A. T., Smith, M., ... & Lloyd-Jones, D. M. (2012). Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology. Archives of Internal Medicine, 172(10), 789-796.
- Holman, D. M., Ding, H., Guy, G. P., Watson, M., Hartman, A. M., & Perna, F. M. (2018). Prevalence of sun protection use and sunburn and association of demographic and behaviorial characteristics with sunburn among US adults. JAMA Dermatology, 154(5), 561-568.
- Chevance, G., Perski, O., & Hekler, E. B. (2021). Innovative methods for observing and changing complex health behaviors: Four propositions. Translational behavioral medicine, 11(2), 676-685.
A Spotlight on Palliative Care Research
Katherine Ramos, PhD✉; Sean O'Mahony, MD; James Gerhart, PhD; Hailey W. Bulls, PhD; Erin R. Harrell, PhD; Megan Johnson Shen, PhD; Rosario Costas-Muñiz, PhD; Normarie Torres Blasco, PhD; and Laura S. Porter, PhD; Palliative Care SIG

Palliative care research focuses on finding ways to improve quality of life and reduce suffering of people living with serious illness and their family caregivers. Members of the Palliative Care SIG are conducting research in diverse areas, spanning program development, pain management, and development of interventions for underserved populations. Below we highlight exciting and novel projects, each of which takes an interdisciplinary focus, considers health equity, and aims to improve the lives of individuals coping with serious, life-limiting illness.
Sean O’Mahony, MD (Associate Professor at Rush University Medical Center) and Jim Gerhart, PhD (Assistant Professor at Central Michigan University) are developing an interdisciplinary palliative care (PC) training program for healthcare professionals and community leaders in Michigan. A state-level needs analysis is underway to identify regional patterns in social determinants of health and PC access. Thus far, they have identified that more intensive care in the final months of life occurs in counties with other social challenges including violent crime and low social capital. Their goal is to develop a state-wide community of professionals knowledgeable about PC to facilitate education, referral, and resource sharing across Michigan communities.
Hailey W. Bulls, PhD (Assistant Professor at University of Pittsburgh) is a clinician and researcher whose mission is to improve pain management and quality of life in patients with cancer, particularly those with advanced disease. Her efforts include identifying patients at high risk for lasting cancer-related pain with the goal of offering targeted, tailored interventions as early as possible. Currently, she is developing a multi-level intervention to eliminate opioid stigma for patients with cancer and their clinicians.
Erin R. Harrell, PhD (Assistant Professor, Associate of the Alabama Research Institute on Aging) is developing and testing interventions to enhance coping skills and preparation of African American caregivers of patients with cancer-related cognitive impairment (CRCI). Her goal is to better understand the unique challenges African American caregivers face as they deal with CRCI, exploring what they value as being helpful in lessening distress and improving bereavement outcomes.
Megan Johnson Shen, PhD (Associate Professor at Fred Hutchinson Cancer Research Center), Rosario Costas-Muñiz, PhD (Assistant Attending Psychologist at Memorial Sloan-Kettering Cancer Center) and Normarie Torres Blasco, PhD (Postdoctoral Researcher at Ponce Health Sciences University) are teaming up to develop psychosocial interventions specifically adapted for Latinx patients with advanced cancer and their family caregivers. Their efforts include (a) developing and pilot testing a theoretically grounded, tailored culturally competent communication coaching intervention to promote advanced care planning (Dr. Shen); (b) adapting Meaning-Centered Psychotherapy for Latino patients to improve spirituality and quality of life and decrease depression, anxiety, and hopelessness (Dr. Costas-Muñiz), and (c) developing Family Meaning-Centered Psychotherapy for Latinx families to improve patients and caregiver outcomes including spiritual well-being and self-efficacy (Dr. Torres Blasco).
If your research or clinical interests involve patients and families coping with serious illness, we encourage you to contact us about opportunities for collaboration.
Addressing Trauma-Related Multimorbidity: Opportunities for Behavioral Scientists to Integrate Trauma-Informed Lifestyle-Based Interventions into Treatment Plans
Michelle M. Pebole, MA✉ and Katherine S. Hall, PhD✉; Violence & Trauma SIG

Experiencing trauma is linked to a myriad of psychosomatic disorders including post-traumatic stress disorder (PTSD), diabetes, obesity, chronic pain, and cardiovascular disease.1-3 These trauma-related symptoms contribute to poor lifestyle behaviors, including low physical activity, alcohol abuse, increased sedentary behavior, and unhealthy diet.4,5 Individuals who experience high rates of violence and trauma often experience personal and systemic barriers such as stigma, weight prejudice, racism, misogyny, and homophobia when accessing healthcare services.6,7 These considerations make non-pharmacological behavioral interventions a valuable treatment option in this population. Yet, exercise, diet, and other lifestyle-related interventions have yet to be recognized as first-line treatments for PTSD and other trauma-related conditions.
Lifestyle-based interventions for trauma-related conditions enhance mental health outcomes while also improving complementary factors not directly targeted in gold standard treatment approaches. For instance, diet, exercise, and mindfulness-based interventions have been repeatedly shown to improve mental and physical health and improve health-related indicators of chronic disease among people with PTSD.8-11 These lifestyle-based treatments have also been shown to improve social health and wellbeing, strengthen community ties, and encourage participants to become more actively engaged in their own healthcare and seek out other appropriate clinical services. Despite the evidence indicating the efficacy of these interventions, current treatment schemes for trauma-related disorders focus primarily on psychotherapy and often ignore these holistic behavioral treatments.
Integrating lifestyle-based interventions into treatment for trauma-related conditions necessitates interdisciplinary collaboration between healthcare providers and behavioral scientists. Widespread adoption of interdisciplinary teams consisting of diet, exercise, and other lifestyle related professionals into first-line treatments for individuals with PTSD is needed to enhance the wellbeing of those exposed to trauma and violence. Identifying best practices for integration of behavioral services into primary mental healthcare is a necessary first step which requires coordination across medical departments and represents a key gap in medical practice that behavioral scientists are qualified to fill.
A key element of creating accessible behavioral healthcare services for this population is employing trauma-informed practice. Although research into trauma-informed practice is growing in the medical field, understanding trauma informed practices and for implementing lifestyle related interventions for groups at highest risk of trauma like women, gender, racial, and ethnic minorities, and incarcerated persons who have experienced sexual trauma, physical abuse, and psychological abuse is still a significant gap in the behavioral medicine field.
In sum, lifestyle-based interventions represent a low-threat avenue for trauma survivors to improve health and wellbeing. These health promoting interventions may be a necessary first step for trauma survivors to take charge of and advocate for their health. There is substantial opportunity for behavioral scientists to partner with mental health providers to improve health among diverse violence-exposed populations. This necessitates a systemic shift towards a whole-body treatment approach which recognizes the widespread effect of trauma on survivors’ physical and mental health and overall wellbeing. Behavioral scientists working in lifestyle related fields are well suited to help fill these gaps. Future work should identify best practices for integrating these interdisciplinary collaborations in healthcare contexts.
References
- Brewerton TD. Eating disorders, trauma, and comorbidity: focus on PTSD. Eat Disord. 2007 Sep;15(4):285–304.
- Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry. 2009 Jan;66(1):72–80.
- Dichter ME, Cerulli C, Bossarte RM. Intimate partner violence victimization among women veterans and associated heart health risks. Womens Health Issues. 2011 Aug;21(4 Suppl):S190–4.
- van den Berk-Clark C, Secrest S, Walls J, Hallberg E, Lustman PJ, Schneider FD, et al. Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: A systematic review and meta-analysis. Health Psychol. 2018;37(5):407–416.
- Hall KS, Hoerster KD, Yancy WS. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015 Jan 16;37:103–115.
- Substance Abuse and Mental Health Services Administration. SAMHSA’s Conceptof Trauma and Guidance for a Trauma-Informed Approach. HHS. 2014 Jul;14-4884:2–18.
- Pebole MM, Gobin RL, Hall KS. Trauma-informed exercise for women survivors of sexual violence. Transl Behav Med. 2020 Jun 14;11(2):686–691.
- Rosenbaum S, Vancampfort D, Steel Z, Newby J, Ward PB, Stubbs B. Physical activity in the treatment of Post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Res. 2015 Dec 15;230(2):130–136.
- Pebole MM, Hall KS, Gobin RL. Physical Activity to Address Multimorbidity among Survivors of Sexual Violence: A Comprehensive Narrative Review. Psychol Sport Exerc. 2021 May;101962.
- Taylor J, McLean L, Korner A, Stratton E, Glozier N. Mindfulness and yoga for psychological trauma: systematic review and meta-analysis. J Trauma Dissociation. 2020 Dec;21(5):536–573.
- Firth J, Marx W, Dash S, Carney R, Teasdale SB, Solmi M, et al. The Effects of Dietary Improvement on Symptoms of Depression and Anxiety: A Meta-Analysis of Randomized Controlled Trials. Psychosom Med. 2019 Apr;81(3):265–280.
New Articles from Annals of Behavioral Medicine and Translational Behavioral Medicine
SBM's two journals, Annals of Behavioral Medicine and Translational Behavioral Medicine: Practice, Policy, Research (TBM), continuously publish online articles, many of which become available before issues are printed. Three recently published Annals and TBM articles are listed below.
SBM members who have paid their 2021 membership dues are able to access the full text of all Annals and TBM online articles via the SBM website by following the steps below.
- Go to the Members Only section of the SBM website.
- Log in with your username and password.
- Click on the Journals link.
- Click on the title of the journal which you would like to electronically access.
To check your membership status, or if you are having trouble accessing the journals online, please contact the SBM national office at info@sbm.org or (414) 918-3156.
Annals of Behavioral Medicine
Chelsea L Ratcliff, PhD, Bob Wong, PhD, Jakob D Jensen, PhD, Kimberly A Kaphingst, ScD
Background
Precision medicine research depends upon recruiting large and diverse participant cohorts to provide genetic, environmental, and lifestyle data. How prospective participants react to information about this research, including depictions of uncertainty, is not well understood.
Purpose
The current study examined public responses to precision medicine research, focusing on reactions toward (a) uncertainty about the scientific impact of sharing data for research, and (b) uncertainty about the privacy, security, or intended uses of participant data.
Methods
U.S. adults (N = 674; 51.9% male; 50% non-Hispanic white; Mage = 42.23) participated in an online experimental survey. Participants read a manipulated news article about precision medicine research that conveyed either certainty or uncertainty of each type (scientific, data). Participants then rated their attitudes toward the research, trust in the researchers, and willingness to join a cohort. We tested direct and mediated paths between message condition and outcomes and examined individual characteristics as moderators.
Results
Overall attitudes were positive and a majority of participants (65%) reported being somewhat or very likely to participate in precision medicine research if invited. Conveying uncertainty of either type had no overall main effect on outcomes. Instead, those who reported perceiving greater uncertainty had lower attitudes, trust, and willingness to join, while those with more tolerance for uncertainty, support for science, and scientific understanding responded favorably to the scientific uncertainty disclosure.
Conclusions
Findings suggest responses to precision medicine research uncertainty are nuanced and that successful cohort enrollment may be well-supported by a transparent approach to communicating with prospective participants.
Lara J LaCaille, PhD, Stephanie A Hooker, PhD, Elaine Marshall, MA, Rick A LaCaille, PhD, Rhea Owens, PhD
Background
The COVID-19 pandemic has resulted in unprecedented disruptions, restrictions, and concerns about physical and mental health. Emerging adulthood, including the first year of college, is associated with declines in healthy eating and physical activity, as well as possible heightened distress. The impact of COVID-19 may exacerbate these concerns.
Purpose
The purpose of this study was to examine changes in health behaviors and perceived stress in emerging adults over the first year of college and to determine whether prepandemic health behaviors were protective for mental health and stress during the initial changes after the COVID-19 pandemic.
Methods
First-year college students (N = 234, 58.6% female) completed three surveys during their first year of school, the third being after the onset of COVID-19 and during a stay-at-home order. At Time 3, we also assessed symptoms of anxiety and depression.
Results
Using linear mixed modeling, sedentary time increased and physical activity decreased over time, but 20%–35% of students reported improvements in these behaviors. Dietary changes appeared mixed, with some improvements noted early during COVID-19. Perceived stress increased over time. Multiple regression indicated that of the health behaviors examined for protective effects on mental health and stress during the pandemic, only diet quality emerged as a significant predictor.
Conclusions
Although notable declines in some health habits were observed over time, including following COVID-19 disruptions, some students reported improved health behaviors. Efforts should be directed at identifying and intervening with students most at risk for poor functioning.
Tamar Goldenberg, PhD, MPH, Kristi E Gamarel, PhD, Sari L Reisner, ScD, Laura Jadwin-Cakmak, MPH, Gary W Harper, PhD, MPH
Background
Transgender and other gender diverse (TGD) youth of color experience stigma within healthcare. Gender affirmation can be a resilience resource; however, little is known about gender affirmation within healthcare.
Purpose
This study explores TGD youth of color’s experiences of stigma and gender affirmation across the entire healthcare experience and their role on motivation to seek care.
Methods
In 2015, cross-sectional surveys and individual in-depth interviews were conducted among 187 TGD youth ages 16–24 living in 14 U.S. cities. Analyses followed a mixed-methods design whereby 33 participants were purposively selected for a qualitative phenomenological analysis based on quantitatively reported gender affirmation needs. Subsequent quantitative analyses examined how healthcare use differed by access to gender affirmation.
Results
Participants qualitatively described experiencing stigma across multiple healthcare settings (e.g., primary care, emergency care, medical gender affirmation), including before (finding providers, scheduling), during (waiting rooms, provider interactions), and after (pharmacy) healthcare visits. Participants who quantitatively reported access to gender-affirming healthcare still described negative healthcare experiences, either because they accessed multiple healthcare services or because of prior negative experiences. Stigma and gender affirmation (both inside and outside of healthcare) influenced motivation to seek care, with variation depending on the type of care. Quantitative analyses confirmed these findings; access to gender affirmation differed for participants who delayed primary care vs. those who did not, but did not vary based on participants’ use of medical gender affirmation.
Conclusions
Findings highlight the importance of promoting gender-affirming healthcare environments to increase access to care for TGD youth of color.
Translational Behavioral Medicine
Rebekah Levine Coley, Christopher F Baum
The COVID-19 pandemic has led to rising morbidity, mortality, and social and economic disruption, likely impairing mental health. The purpose of this study was to track trends in mental health symptoms, use of services, and unmet need for services among U.S. adults and to delineate variation across demographic strata. Data were drawn from the 2020 U.S. Household Pulse Survey from repeated cross-sectional online surveys collected between April 23 and November 23, 2020 from 1,483,378 US adults, weighted to represent the U.S. population. Survey respondents self-reported their symptoms of anxiety and depression, use of medication, counseling services, and unmet need for services. Reports of probable anxiety and depression rose significantly through the study period, to prevalence rates of 50% and 44%, respectively, by November 2020, rates six times higher than early 2019 U.S. norms. Use of prescription medication, counseling services, and unmet need for mental health services also rose significantly. Prevalence rates of probable mental health disorders were highest among young, less educated, single, female, Black and Hispanic respondents, with age and education disparities growing over cohorts. Young, female, and moderately educated respondents also reported higher unmet needs for services. Disparities in estimates of mental health disorders and mental health treatment indicate a striking disequilibrium between the potential need for and the use of mental health services during the COVID-19 pandemic. Rising mental health challenges are being borne largely by young, less advantaged people of color and women, with the potential for expanded interruptions to optimal functioning and societal recovery from COVID-19.
Claire C Conley, Amy K Otto, Glynnis A McDonnell, Kenneth P Tercyak
Communicating risk and other health information in a clear, understandable, and actionable manner is critical for the prevention and control of cancer, as well as the care of affected individuals and their family members. However, the swift pace of development in communication technologies has dramatically changed the health communication landscape. This digital era presents new opportunities and challenges for cancer communication research and its impact on practice and policy. In this article, we examine the science of health communication focused on cancer and highlight important areas of research for the coming decade. Specifically, we discuss three domains in which cancer communication may occur: (a) among patients and their healthcare providers; (b) within and among families and social networks; and (c) across communities, populations, and the public more broadly. We underscore findings from the prior decade of cancer communication research, provide illustrative examples of future directions for cancer communication science, and conclude with considerations for diverse populations. Health informatics studies will be necessary to fully understand the growing and complex communication settings related to cancer: such works have the potential to change the face of information exchanges about cancer and elevate our collective discourse about this area as newer clinical and public health priorities emerge. Researchers from a wide array of specialties are interested in examining and improving cancer communication. These interdisciplinary perspectives can rapidly advance and help translate findings of cancer communication in the field of behavioral medicine.
Chanita Hughes Halbert, Caitlin G Allen
Achieving health equity among disparity populations has been a national, regional, and local priority for several years. Health promotion and disease prevention behaviors play an important role in achieving health equity; the first generation of behavioral science studies in minority health and health disparities have provided important insights about the nature and distribution of risk exposure behaviors in disparity populations. Interventions have also been developed to enhance health promotion and disease prevention behaviors using behavioral counseling, tailored health communications, and interventions that are developed collaboratively with community stakeholders. Although intervention development and evaluation are components of transdisciplinary translational behavior research, discovery science is a critical first step in translational research. Consistent with this, conceptual models and frameworks of minority health and health disparities have evolved to include multilevel determinants that include basic behavioral mechanisms such as stress responses and stress reactivity that have physiological, psychological, and behavioral components that are relevant to minority health and health disparities. This report describes priorities, opportunities, and barriers to conducting transdisciplinary translational behavioral research during the next generation of minority health and health disparities research.
Honors and Awards
Congratulations to the following Society of Behavioral Medicine (SBM) members who recently received awards or were otherwise honored. To have your honor or award featured in the next issue of Outlook, please email aschmidt@sbm.org.
Amy L. Ai, PhD
The International Society for Traumatic Stress Studies honored Dr. Ai with its 2021 Innovation Award.
Norman B. Anderson, PhD
As part of its High-Risk, High-Reward Research Program, NIH selected Dr. Anderson for a 2021 Director's Transformative Research Award.
Linda E. Carlson, PhD
Dr. Carlson received the 2021 Alberta Oncology Research Excellence Award.
Linda S. Ehrlich-Jones, PhD, RN, ACNS-BC, FAAN
Dr. Ehrlich-Jones was recently awarded Fellow status by the American Academy of Nursing.
Martin S. Hagger, PhD
Dr. Hagger was recognized with a Clarivate Web of Sciences Highly Cited Researcher Award for 2021
Abby King, PhD; Patricia Rodriguez Espinosa, PhD; Lisa Goldman Rosas, PhD; and Michele Lanpher Patel, PhD
Stanford University selected the Stanford Our Voice Research Initiative for one of its 2021 Integrated Strategic Plan Star Awards.
Nikos Ntoumanis, PhD
Dr. Ntoumanis was recently elected a Fellow of the Society for Health Psychology (APA Division 38).
Members in the News
The following SBM members and their research were recently featured in news articles, videos, or journals. To have your news spot featured in the next issue of Outlook, please email aschmidt@sbm.org.
Jamie Faro, PhD
Dr. Faro was quoted in an article published by Medscape Medical News on a text-based COVID-19 monitoring system.
CLASSIFIEDS
University of Kansas Medical Center - Postdoc, Physical Activity and Weight Management
The Division for Physical Activity and Weight Management supports research, training and clinics for the prevention and treatment of obesity in children, adolescents, and adults. Interests include all components of energy balance, metabolic syndrome, weight management delivery systems, technology, brain function, special populations (those with intellectual and physical disabilities), rural populations, medical comorbidities, and others.
Currently, the Division has 7 funded R01 projects from the National Institutes of Health to investigate exercise and nutrition. Since 1986 the Division has maintained an ongoing clinical treatment program termed the Kansas Weight Management Programs designed to provide weight loss and weight maintenance for adults. This program also supports pilot projects that can be used for future major funded research studies. To learn more about the Division grants and publications, please go to our website. Our Division is seeking: Post-Doctoral Fellows.
For further information and/or to apply please go to: https://kumc.wd5.myworkdayjobs.com/kumc-jobs Job Post: JR002437 Questions? Email: kim@ku.edu.
EO/AA
CLASSIFIEDS
Lirio - Head of Behavioral Research
Who We Are:
Lirio is the leader in behavior change AI, combining behavioral science with artificial intelligence to move people to better health. Through Precision Nudging™, our intelligent behavior change journeys assemble and deliver tailored, behavioral interventions to overcome unique barriers to engaging with and acting on health recommendations. By scaling personalized interventions, our clients deliver patient-focused experiences that initiate and drive sustained behaviors across their entire population, optimizing patient engagement, closing gaps in care, lowering costs, and measurably improving health outcomes.
Who You Are:
You’re passionate about transforming people’s health through technology. You’re looking to be part of a dynamic organization that moves quickly, where you can learn and grow and work alongside colleagues to develop and improve our solutions. You have a growth mindset and seek progress over perfection.
What You’ll Be Doing:
The Head of Behavioral Research is responsible for Lirio’s behavioral research and behavioral insights portfolio. The role will lead a team and execute alongside them to scientifically evaluate, improve, and validate Lirio’s Precision Nudging solutions and generate meaningful, behavioral insights. The Head of Behavioral Research will work collaboratively and crossfunctionally to deliver rigorous quantitative and qualitative research results, continuous scientific output, and meaningful insights for clients, prospects, and investors. The role is responsible for translating insights and results into actionable recommendations for Lirio’s functional area leads and Executives, and credibility in the marketplace and scientific community, respectively. The role requires working in a fast-paced, highly collaborative environment, and a strong ability to go deep into the details, back up to 30,000 feet and everywhere in between. The position can be located remotely and reports directly to Lirio’s Chief Behavioral Officer.
Additional Responsibilities:
- Closely collaborate with Lirio’s mid- and senior-level scientists on research innovations and evaluations
- Build and lead a team of behavioral researchers and behavioral data scientists
- Lead the delivery of complex, insight-driven results to clients, prospects, and investors
- Publish peer-reviewed scientific papers and present peer-reviewed results at conferences that serve both scientific and business objectives
- Grow Lirio’s behavioral science credibility and industry thought leadership
- Lead and co-create innovative and pragmatic behavioral research and insights requirements to drive product improvements
- Partner/consult with functional area leaders and colleagues across all departments to ensure alignment of behavioral research and insights activities
- Oversee/support research study design and data interpretation by internal and external research collaborators
Required Qualifications:
- Doctoral degree in an applied behavioral science field (e.g., behavioral economics, social psychology, health psychology, public health, behavioral/health informatics)
- Demonstrated expertise and thought leadership in digital health, health communication, and/or behavior change
- 5-10 years of experience leading randomized controlled trials as Principal Investigator
- 10+ years of experience leading and collaborating on soup-to-nuts prospective and retrospective research
- Exceptionally strong qualitative, quantitative, mixed methods, written and oral communication skills
- Strong track record of peer-reviewed publications and presentations at professional conferences
- Experience validating the accuracy, relevance, timeliness, and scientific soundness of data analyses plans and results
- Experience communicating research activities and results to a variety of audiences (e.g., nonscientific stakeholders, clinical decision makers, or to inform business decisions)
- Experience hiring, growing, and retaining high-performing researchers and research staff
- Experience fostering a strong team culture of transparency and cross-functional collaboration
- Solid organizational skills, including attention to detail and an ability to lead multiple projects and initiatives simultaneously
- Excellent statistical software, qualitative software, and Microsoft Office skills
Nice to Have Skills:
- Prior experience working in a business environment / working in a startup a plus
- Thrives in a fast-paced environment, flexible to adapt to change, creative problem solver
- Positive, win together, growth mindset
Perks:
- Competitive compensation and profit-sharing plan
- Developmental opportunities to grow your career
- Comprehensive benefit package 401K matching (immediately vested)
- Flexible/Unlimited PTO
- 10 Paid Holidays
- Strong emphasis on work-life balance
Visit our website to learn more and apply.
CLASSIFIEDS
Rutgers University - Endowed Chair, Oncology Nursing
The Rutgers School of Nursing invites applications for the position of Rutgers Biomedical Health Sciences Endowed Chair in Oncology Nursing. This exciting position offers a highly competitive, internal funding package for research expansion, and the opportunity for a joint appointment at the Rutgers Cancer Institute of New Jersey. Located on the New Brunswick campus, the comprehensive Cancer Institute of New Jersey is the first and only NCI-designated cancer institute in the state.
The successful candidate will be a senior level PhD-prepared researcher with a record of externally funded and oncology-related research, expertise in oncology nursing, and experience in academic and clinical settings. The goal of this endowment is to advance oncology nursing research, education, and evidence-based practices. The Chair will work collaboratively with nursing colleagues and colleagues from other disciplines. Rutgers School of Nursing is located within a comprehensive research-focused university, offers degrees ranging from pre-licensure nursing to the PhD in Nursing, and is a member of one of the most comprehensive academic health centers in the nation. The position will report directly to the Associate Dean of Nursing Science.
Minimum Qualifications:
- An earned a research-focused doctorate in nursing or related field.
- A demonstrated record of NIH funding or NIH-equivalent funding.
- A distinctive record of teaching, high impact publications, and other scholarly activities.
- Academic and clinical experience in the arena of oncology nursing.
- Eligible for tenure at Rutgers School of Nursing, Rutgers Biomedical Health Sciences.
- Current funding award from NIH or equivalent.
- Eligible for RN licensure in the state of New Jersey
The School of Nursing is one of eight schools that comprise Rutgers Biomedical and Health Sciences. As part of Rutgers Biomedical and Health Sciences, the School of Nursing (Newark) offers unique opportunities in education, research, and practice at a leading national research university which is New Jersey’s preeminent comprehensive public institution of higher education.
Innovative academic offerings include bachelor’s, master’s, post-master’s, doctor of nursing practice (DNP), and doctor of philosophy (PhD) programs that prepare nurse leaders of today and tomorrow at campus locations in Newark, New Brunswick, and Blackwood, NJ.
As one of the nation’s largest, most comprehensive nursing schools, Rutgers School of Nursing is dedicated to the pursuit of excellence in education, evidence-based research and health care delivery, and promotion of community health. The school is dedicated to meeting the educational needs of current and future students through innovative teaching and learning strategies in the undergraduate and graduate programs. The DNP Program at Rutgers School of Nursing is one of the largest in the United States, making Rutgers School of Nursing one of the most significant educators of DNP-prepared nurses in the world.
Rutgers University School of Nursing is ranked in 2021 US News and World Report as No. 19 (tie) in Best Nursing Schools: Master’s and No. 15 (tie) in Best Nursing Schools: Doctor of Nursing Practice.
Contact Christine Duggan at christine.duggan@rutgers.edu or 973.353.0637 or follow this link to apply: https://jobs.rutgers.edu/postings/139746




 QCDs or IRA Charitable Rollover Gifts are tax-free gifts transferred directly from your IRA account to SBM. If you’re over 70 ½ years old, making a QCD is a great option to lower your income taxes while doing good for others. QCDs count toward your Required Minimum Distribution (up to $100,000), effectively lower your adjusted gross income and bring about many tax benefits, including eliminating itemized gifts.2
QCDs or IRA Charitable Rollover Gifts are tax-free gifts transferred directly from your IRA account to SBM. If you’re over 70 ½ years old, making a QCD is a great option to lower your income taxes while doing good for others. QCDs count toward your Required Minimum Distribution (up to $100,000), effectively lower your adjusted gross income and bring about many tax benefits, including eliminating itemized gifts.2